On Sept 3, 1928, Dr. Alexander Fleming accidentally discovered a medicine that altered the course of history. Dr. Fleming was among many scientists researching influenza after the devastating Spanish flu pandemic in 1918. While working with this virus, he began to experiment with other substances. Fleming facilitated an accidental experiment when he left staphylococcus bacteria in a petri dish for an extended period of time. When he came back to his lab, Fleming observed an unusual occurrence. The mold around the bacteria prevented the bacteria from growing. Through this, Dr. Fleming discovered that mold produces a self-defense chemical that kills surrounding bacteria. He named this chemical Penicillin, the first of many antibiotics discovered in the 20th century.
Antibiotics are the reason most of us are alive today. Before the discovery of penicillin, the main causes of death included pneumonia, tuberculosis, and diarrhea. Of these deaths, 40% were children under the age of 5 years old. Things like childbirth, cuts, and even a common cold could be a death sentence for those afflicted. Antibiotics increased the average life expectancy from 47 years old in 1900 to 74 in 2000. Penicillin alone has saved over 500 million lives since its discovery, and continues to combat infection to this day. Antibiotics transformed medicine into a reliable science that everyone depends on.

Antibiotics are required in the US and many other countries before every surgery. This routine is standard practice in today’s world because antibiotics are central to infection prevention and control. A registered surgical nurse, Jen Hughes, explains her use of antibiotics before procedures.
“As a nurse working in the operating room, part of the infection prevention model is giving patients antibiotics prior to us making our surgical incision,” Hughes said. “This allows patients to have better outcomes when it comes to post-op infection.”
Antibiotics are used constantly due to their convenience and availability in most parts of the world. However, antibiotics have their fair share of challenges. The most pressing issue includes the overuse of antibiotics and the strength of bacteria itself. Bacteria are like any other organism, as their primary goal is survival. Through Darwin’s theory of natural selection, we understand that the strongest traits prevail due to reproduction and mutation. Mrs. Alten, Lakewoods AP bio teacher, explains this idea in more detail.
“The bacteria that don’t have the resistance die, and the ones that do have the resistance don’t die, so then they can keep copying and growing and growing,” Alten said. “So then they become the dominant population.”
Natural selection is easy to grasp. All species have had to survive by passing strong traits to the new generation and then continue to pass down helpful mutations. In addition to reproduction, bacteria have an extra method to transfer resistance. Bacteria can pass their resistance to other bacteria using plasmids and pili.
“So we have plasmids which are what carry antibiotic resistance,” Alten said. “Bacteria has its main DNA and then it has these little plasmids. Bacteria can pass that plasmid from one bacteria to another through the pili. So they connect, they make a tube between them, and then they can pass the resistance to one another.”
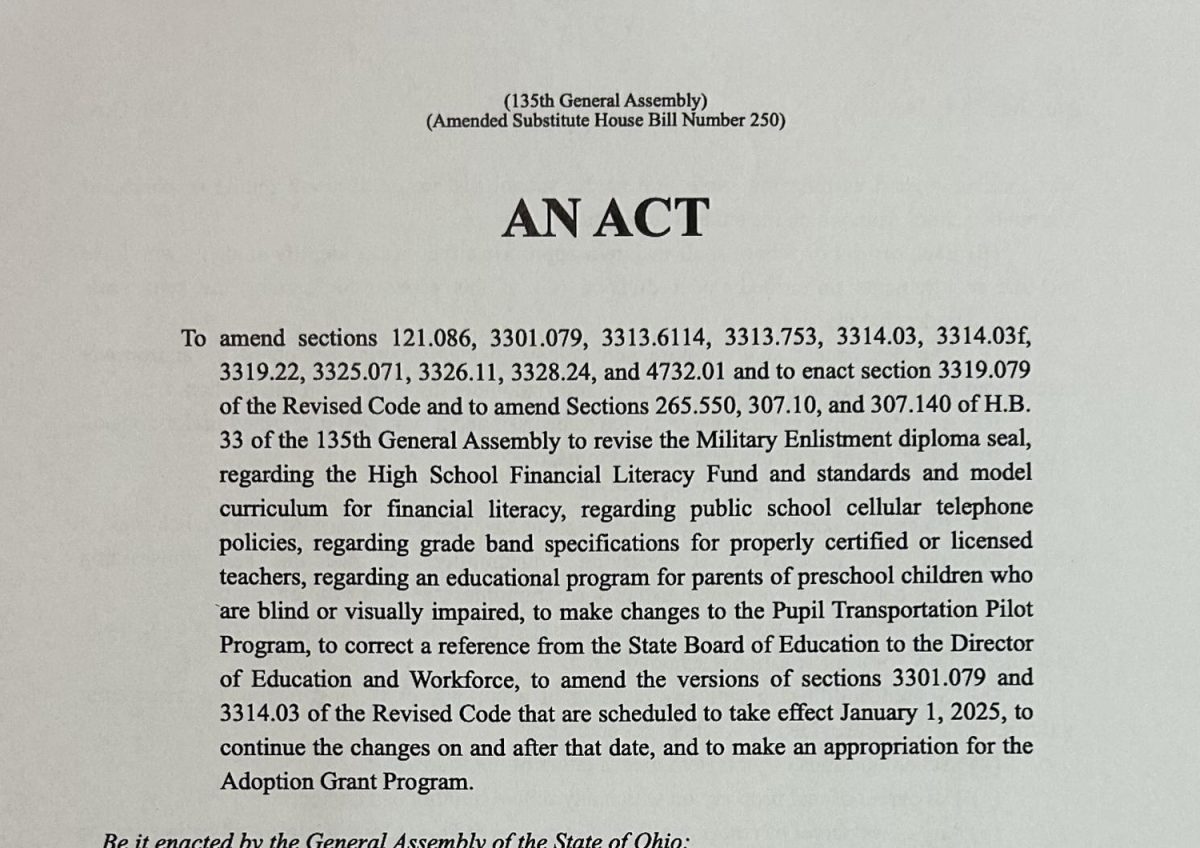
Bacteria can easily pass resistance to other bacteria. This is a huge problem for infected people who rely on antibiotics as a life-saving remedy. Antibiotic resistance is a huge issue in the world today and continues to worsen as more and more bacteria obtain protection. By 2050, scientists predict that antibiotic resistance will be the leading cause of death. This means that in 25 years, antimicrobial resistance will claim more lives than gun violence, car accidents, and even cancer.
Resistance is exponential. As more resistant bacteria reproduce, there are more opportunities for passing resistance through plasmids. Due to this growth, antimicrobial bacteria have become an issue in recent years.

“On a global scale, the problem of antibiotic resistance is pretty big,” Alten said.
And with time, this issue is projected to increase unless another solution is created. Board-certified podiatrist Dr. Kovach highlighted the changes she has seen throughout her practice.
“I have been in practice for 28 years, and I would say, probably over the past 10 years, I’ve noticed more of a resistance to the normal antibiotics that I usually use,” Dr. Kovach said.
This rise in resistance is in part due to overuse and uncontrolled distribution in hospitals. Bacteria can gain resistance when they are exposed to unneeded antibiotics.
“Taking unnecessary antibiotics doesn’t give you your own infection, but what it doesn’t do is help your symptoms get better,” Dr. Kovach said. “It exposes your body to antibiotics when it doesn’t need it, and it allows, with frequency, your body to develop resistance. If we are thinking about resistance, antibiotics, and resistance, what we don’t want to do is take antibiotics all the time because then the more resistant you will be.”
Nurse Jen Hughes describes the measures hospitals and patients need to take to combat this overuse.
“When patients are given an antibiotic, they need to take their antibiotic until it’s completely gone, even if they start to feel better, and prevention is truly key,” Hughes said. “So eating healthy, exercising, and washing your hands, those are probably three of the best things that you can do to your body to fight infection.”
Avoiding infection to save antibiotics for when they are truly necessary is one of the best ways to fight overuse. Doctors must make the right decisions when prescribing the medication and avoid prescribing it to patients unless they truly need it. If you are introduced to an antibiotic before it is required, the bacteria in your body will become immune due to bacteria’s constant mutation and natural selection. Antibiotics save many lives. In order for them to continue having this effect, we need to limit their unnecessary consumption.